The intricate relationship between the gut and the brain has garnered significant attention in recent years, leading to a burgeoning field of research known as psychobiotics. This term encapsulates the idea that the gut microbiome—the vast community of microorganisms residing in our digestive tract—can influence mental health and emotional well-being. The gut-mood connection is not merely a theoretical concept; it is supported by a growing body of evidence suggesting that the state of our gut can have profound effects on our mood, anxiety levels, and overall mental health.
This connection is particularly relevant in an era where mental health issues are on the rise, prompting scientists and healthcare professionals to explore innovative approaches to treatment that consider the gut as a pivotal player in emotional regulation. Understanding the gut-mood connection requires a multidisciplinary approach, integrating insights from microbiology, neuroscience, psychology, and nutrition. The implications of this relationship are vast, suggesting that interventions aimed at improving gut health could potentially serve as adjunct therapies for mood disorders.
As we delve deeper into this topic, it becomes clear that the gut is not just a passive organ involved in digestion; it is an active participant in our emotional landscape, influencing how we feel and respond to the world around us.
The Role of Gut Microbiota in Mood Regulation
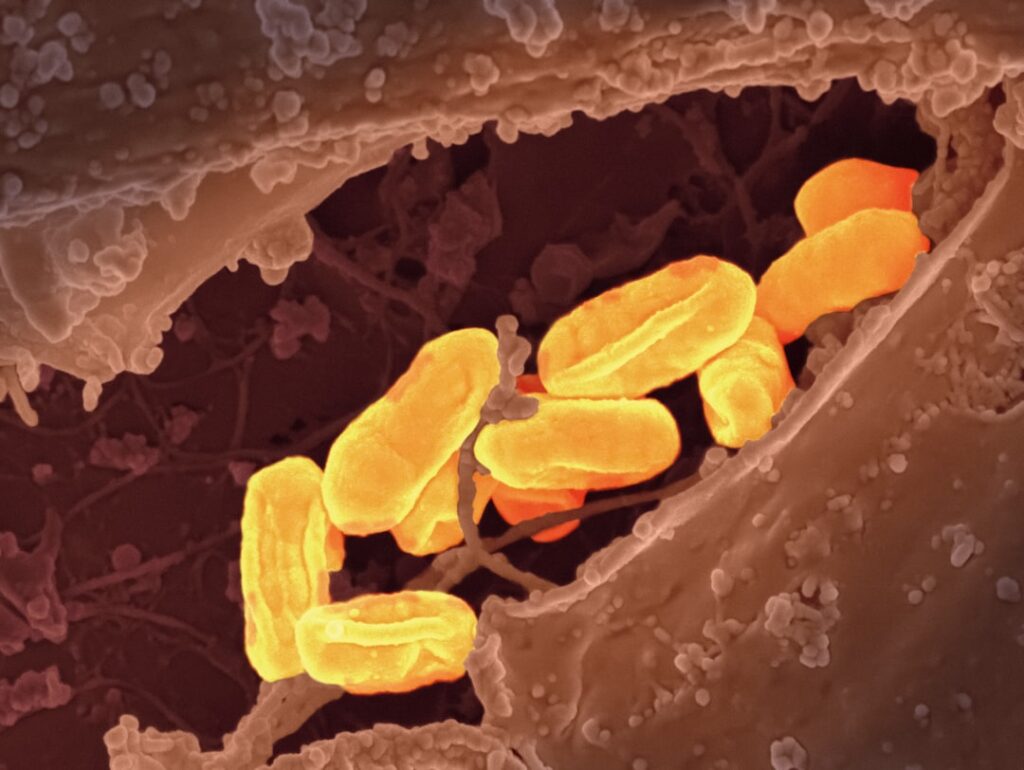
Gut microbiota refers to the trillions of microorganisms, including bacteria, viruses, fungi, and archaea, that inhabit our intestines. These microbes play a crucial role in various bodily functions, including digestion, metabolism, and immune response. However, their influence extends far beyond mere physical health; emerging research indicates that gut microbiota can significantly impact mood regulation.
For instance, certain strains of bacteria have been linked to the production of neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), both of which are essential for maintaining emotional balance. In fact, it is estimated that about 90% of serotonin is produced in the gut, underscoring the importance of gut health in mood regulation. Moreover, studies have shown that individuals with depression or anxiety often exhibit altered gut microbiota profiles compared to those with stable mental health.
For example, a study published in the journal “Nature Microbiology” found that individuals with major depressive disorder had lower levels of certain beneficial bacteria, such as Lactobacillus and Bifidobacterium. These findings suggest that a diverse and balanced gut microbiome may be protective against mood disorders. Furthermore, animal studies have demonstrated that transferring gut microbiota from healthy mice to those exhibiting depressive behaviors can alleviate symptoms, providing compelling evidence for the role of gut bacteria in mood regulation.
The Impact of Diet on Gut Health and Mood

Diet plays a pivotal role in shaping the composition and diversity of gut microbiota. The foods we consume can either nourish beneficial bacteria or promote the growth of harmful pathogens. Diets rich in fiber, fruits, vegetables, and fermented foods have been shown to support a healthy microbiome, while high-sugar and high-fat diets can lead to dysbiosis—a state of microbial imbalance that has been associated with various health issues, including mood disorders.
For instance, a diet high in processed foods may lead to an overgrowth of pro-inflammatory bacteria, which can contribute to feelings of anxiety and depression. The Mediterranean diet serves as an exemplary model of how dietary choices can influence both gut health and mood. Characterized by an abundance of fruits, vegetables, whole grains, legumes, nuts, and healthy fats such as olive oil, this diet has been linked to lower rates of depression and anxiety.
Research has shown that individuals adhering to a Mediterranean diet exhibit higher levels of beneficial gut bacteria and lower levels of inflammatory markers associated with mood disorders. Additionally, fermented foods like yogurt, kefir, sauerkraut, and kimchi are rich in probiotics that can enhance gut health and potentially improve mood by promoting a balanced microbiome.
The Gut-Brain Axis: How the Gut Communicates with the Brain
| Aspect | Metrics |
|---|---|
| Microbiota Composition | Diversity of gut bacteria |
| Neurotransmitters | Levels of serotonin, dopamine, and GABA |
| Immune System | Cytokine levels |
| Intestinal Permeability | Measurement of zonulin levels |
| Brain Function | Neuroimaging data |
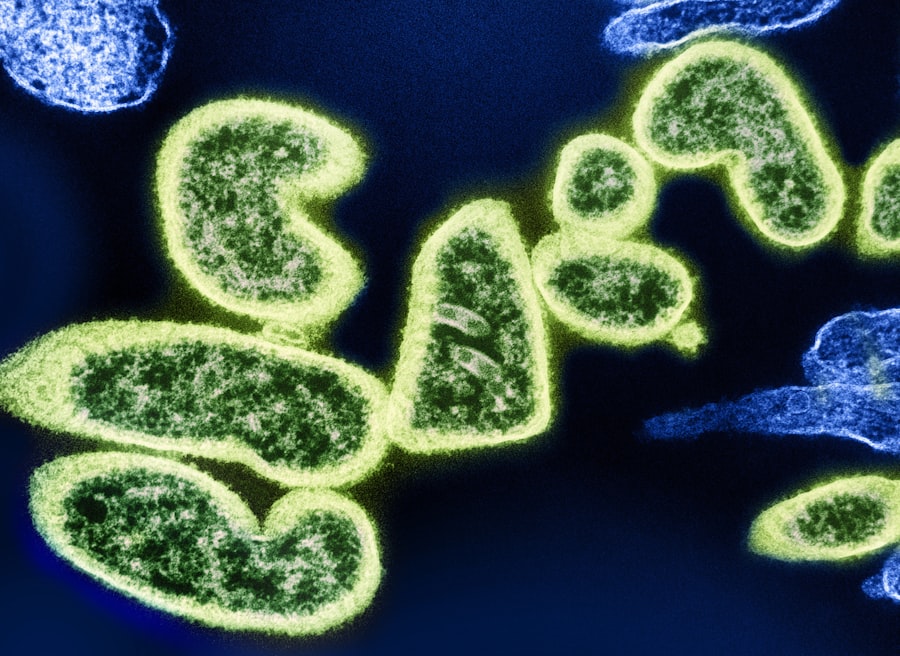
The gut-brain axis refers to the bidirectional communication network between the gastrointestinal tract and the central nervous system. This complex system involves neural pathways, hormonal signals, and immune responses that allow the gut to communicate with the brain and vice versa. One of the primary pathways for this communication is through the vagus nerve, which serves as a major conduit for transmitting signals between the gut and the brain.
When the gut microbiota produce metabolites such as short-chain fatty acids (SCFAs), these compounds can influence brain function by modulating neurotransmitter production and reducing inflammation. Research has demonstrated that alterations in gut microbiota can lead to changes in behavior and mood. For example, studies involving germ-free mice—those raised without any gut bacteria—have shown that these animals exhibit increased anxiety-like behaviors compared to their conventionally raised counterparts.
When researchers introduced specific strains of beneficial bacteria into these germ-free mice, they observed a reduction in anxiety behaviors, highlighting the potential for gut microbiota to influence emotional states through the gut-brain axis. This intricate interplay suggests that maintaining a healthy gut environment may be crucial for optimal brain function and emotional well-being.
The Influence of Stress on Gut Health and Mood
Stress is a well-known factor that can adversely affect both gut health and mood. Chronic stress can lead to alterations in gut microbiota composition, increased intestinal permeability (often referred to as “leaky gut”), and heightened inflammation—all of which can contribute to mood disorders. When an individual experiences stress, the body releases stress hormones such as cortisol, which can disrupt the delicate balance of gut bacteria.
This dysbiosis can exacerbate feelings of anxiety and depression, creating a vicious cycle where poor gut health further intensifies stress responses. Moreover, stress can also impact dietary choices, leading individuals to gravitate toward unhealthy comfort foods that may further compromise gut health. For instance, during periods of high stress, people may consume more sugary or fatty foods as a coping mechanism.
This dietary shift can negatively affect gut microbiota diversity and promote inflammation, ultimately influencing mood negatively. Understanding this relationship underscores the importance of stress management techniques—such as mindfulness practices, exercise, and adequate sleep—in maintaining both gut health and emotional well-being.
Gut Health and Mental Health Disorders
The link between gut health and mental health disorders is becoming increasingly evident in clinical research. Conditions such as depression, anxiety disorders, bipolar disorder, and even schizophrenia have been associated with dysbiosis or imbalances in gut microbiota. For instance, individuals with irritable bowel syndrome (IBS), a condition characterized by gastrointestinal distress, often report higher rates of anxiety and depression compared to those without IBS.
This correlation suggests that gastrointestinal symptoms may be intertwined with psychological distress. Furthermore, emerging studies are exploring how specific interventions targeting gut health could serve as adjunctive treatments for mental health disorders. Probiotic supplementation has shown promise in alleviating symptoms of depression and anxiety in some clinical trials.
A meta-analysis published in “Psychological Medicine” found that probiotics could significantly reduce depressive symptoms among participants compared to placebo groups. These findings highlight the potential for harnessing the power of gut microbiota modulation as a therapeutic strategy for improving mental health outcomes.
Strategies for Improving Gut Health and Mood
Improving gut health is a multifaceted endeavor that encompasses dietary changes, lifestyle modifications, and possibly supplementation with probiotics or prebiotics. A diet rich in fiber from fruits, vegetables, whole grains, legumes, nuts, and seeds can promote a diverse microbiome by providing essential nutrients for beneficial bacteria. Incorporating fermented foods into one’s diet can also enhance microbial diversity while introducing live probiotics that support gut health.
In addition to dietary strategies, lifestyle factors play a crucial role in maintaining gut health. Regular physical activity has been shown to positively influence gut microbiota composition while reducing stress levels—both of which are beneficial for mood regulation. Furthermore, practicing stress-reduction techniques such as yoga or meditation can help mitigate the negative effects of stress on both gut health and emotional well-being.
Adequate sleep is another critical component; poor sleep quality has been linked to dysbiosis and increased susceptibility to mood disorders.
Future Directions in Gut-Mood Research
As research into the gut-mood connection continues to evolve, several exciting avenues are emerging for future exploration. One area of interest is personalized nutrition based on individual microbiome profiles. By understanding how specific dietary components interact with an individual’s unique microbiota composition, tailored dietary recommendations could be developed to optimize both gut health and mental well-being.
Another promising direction involves investigating the potential therapeutic applications of psychobiotics—probiotics specifically designed to improve mental health outcomes. Clinical trials exploring various strains of probiotics for their effects on mood disorders are underway, with researchers aiming to identify which specific bacteria may confer benefits for different populations. Additionally, there is growing interest in understanding how environmental factors—such as exposure to antibiotics or changes in lifestyle—affect the microbiome over time and subsequently influence mental health trajectories.
As we deepen our understanding of these complex interactions between diet, microbiota, stress, and mental health disorders, we may uncover novel strategies for prevention and treatment that harness the power of our gut to enhance emotional well-being.
FAQs
What is gut health?
Gut health refers to the balance of microorganisms that live in the digestive tract. A healthy gut microbiome is essential for proper digestion, nutrient absorption, and overall well-being.
How does gut health affect mood?
Research suggests that the gut microbiome can influence brain function and behavior through the gut-brain axis. Changes in the gut microbiota have been linked to mood disorders such as anxiety and depression.
What factors can impact gut health?
Diet, stress, antibiotics, and other medications can all affect the balance of bacteria in the gut. Consuming a diverse range of fiber-rich foods, managing stress, and avoiding unnecessary antibiotic use can support a healthy gut microbiome.
What does the science say about the connection between gut health and mood?
While there is growing evidence to support the link between gut health and mood, more research is needed to fully understand the mechanisms involved. Some studies have shown that probiotics and prebiotics may have a positive impact on mood, but the results are not yet conclusive.
Can improving gut health help improve mood?
While there is no guarantee that improving gut health will directly improve mood, maintaining a healthy gut microbiome through a balanced diet and lifestyle may contribute to overall well-being. It is important to consult with a healthcare professional for personalized advice.